Despite what many have been led to believe, dairy does not do a body good. In fact, increased bone fractures and osteoporosis directly correlate with increased dairy consumption — the more dairy, the more bone fractures. Although the prevailing sentiment is that consuming cow’s milk reduces the risk of osteoporosis, in fact, it does just the opposite.[1]
Cow’s milk does contain calcium, but that isn’t the end of the story. Any value from the calcium in the cow’s milk is outweighed by the negative impacts from dairy.
Science shows that increased consumption of high protein-foods like milk and other animal derived foods (coupled with consumption of less plant derived foods) are associated with lower long-term bone health.
“I tell my patients, including (parents of) children, that drinking milk will NOT make bones stronger, positively affect bone growth, prevent bone fractures, or hasten fracture healing. This is based on my 35 years of orthopedic surgery practice and experience.”
— Orthopedist Tedd L. Weisman, MD, FAAOS, Connecticut Orthopaedics, Attending Orthopedic Surgeon, Yale New Haven Health System
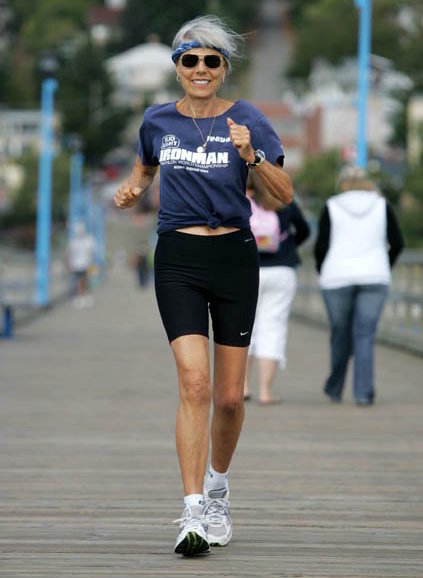
Ruth Heinrich has participated in six Ironman Triathlons since ditching dairy in the 1980s!

The good news is that by consuming a plant-based diet we can increase our calcium consumption while simultaneously protecting the calcium in our bones. The recommended daily allowance (RDA) for calcium is 1,000 mg/day.[2] This RDA can easily be met by eating a salad of spinach (3 cups 735 mg), chickpeas (½ cup 54 mg), broccoli (½ cup 31 mg), and tofu (½ cup 434 mg). Other rich sources of calcium include collards (1 cup 268 mg), kale (1 cup 94 mg), mustard greens (1 cup 165 mg), swiss chard (1 cup 102 mg), black beans (1 cup 102 mg), and white beans (1 cup 161 mg). You can also get calcium through fortified orange or apple juices (300 mg per cup) and fortified plant-based milks (450-560 mg per cup).
Beyond the widespread misunderstanding of dairy’s connection with calcium and strong bones, many also believe that cows milk is a crucial source of vitamin D. But this is another myth. Vitamin D is crucial for calcium absorption — the process of mineralization and strengthening of bone. However, the vast majority of the vitamin D we use (90%) is made by our own bodies via exposure to sunlight; less than 10% comes from food. When our skin is exposed to sunlight, our body turns cholesterol already flowing in our bloodstream into vitamin D.[3] This vitamin D is inactive until it passes through the liver and kidneys, whereupon it becomes active and facilitates the absorption of calcium in the GI tract. When vitamin D levels are insufficient, calcium absorption is at risk of being insufficient, and can lead to osteoporosis.
“Cows are no better at making vitamin D than we are. Vitamin D is added in the processing of milk, after its extraction from the cow. In other words, cow’s milk, soy milk, and almond milk are all fortified with vitamin D.”
The best way to get vitamin D is from sunlight, but it is also important to eat foods[4] such as mushrooms and vitamin D fortified plant-based cereals and milks. For those with inadequate sun exposure (e.g., winter months), a vitamin D supplement may be valuable.[5] Our vitamin D requirement is between 1,000 IU and 2,000 IU per day, depending on such factors as sun exposure (Northerners need more), age (the elderly need more), medical history (those with GI problems need more), and diet (those with nutritionally poor diets need more).
An important 2014 Swedish study[6] of over 100,000 men and women showed an inverse relationship between milk consumption and both life expectancy and fracture incidence. Greater milk consumption was associated with a higher mortality and fracture rate. Indeed, various population studies in the U.S.[7, 8, 9, 10] and elsewhere[11, 12, 13] that analyzed the relationship between dietary calcium intake and fractures have failed to show that high calcium intakes (primarily from dairy) protect against fractures.[14]
“We have had evidence for well over a hundred years that animal protein decreases bone health, and yet we still are warned almost daily about our need for dairy to provide calcium for strong bones. The science is clear — ditch the dairy for stronger bones.” — T. Colin Campbell, PhD.

85-year-old Dr. T. Colin Campbell
out for his daily run
Help us get the word out about the association between dairy and acne. Check out our media kit to get started!
5 TIPS FOR DITCHING DAIRY TODAY
START TRANSITIONING TO WFPB with the help of this Toolkit! For example, the info sheet WFPB Grocery Basics lists common ingredients found in WFPB recipes – most of which can be purchased at chain grocery stores.
JOIN OR START A LOCAL WFPB GROUP for support getting started on your whole food, plant-based (WFPB) journey. Becoming part of the PlantPure Communities Pod Network opens the door to encouragement, education, and networking opportunities.
TRY A SAMPLE COURSE from the T. Colin Campbell Center for Nutrition Studies in partnership with eCornell and learn how to apply a whole food, plant-based lifestyle to improve your health.
FOCUS ON EXERCISE TO STRENGTHEN YOUR BONES: Creating strong bones is not just a matter of swallowing calcium-rich foods. Just like muscles that need to be repeatedly used to make them stronger, our bones need to be used daily through gentle, sustained weight-bearing exercise, so the osteoblast cells in our skeleton will be stimulated to lay down new bone matrix.[15] This is covered extensively in Dr. Michael Klaper’s video on “Healthy Bones.”
GET COOKING: Try these delicious dairy-free dishes that provide calcium and vitamin D.
Mushroom Stroganoff
This creamy mushroom sauce is loaded with flavor, and the soy milk and mushrooms provide excellent sources of calcium and Vitamin D. You can experiment with many different kinds of mushrooms in this dish – they all work well.
Buddha Bowl
This recipe is easy to make for any meal. The quinoa, kale, broccoli and chickpeas are great sources of calcium. The sauce can make or break a Buddha bowl, and this sauce is amazing!
Sweet Pepper Coconut Corn Chowder
This soup is a favorite of the PlantPure Communities staff! The chickpeas provide an excellent source of plant-based calcium. Serve this colorful dish with brown rice or a baked potato with a mixed green salad for a perfect meal.
Buffalo Beans and Greens
This delicious and fun recipe is packed full of calcium and has so many flavors and textures! The Blue Cheez Dressing is sure to be a hit – you may want to make double the sauce so you can use it on other vegetables throughout the week!
*In writing this article, PlantPure Communities (PPC) consulted with T. Colin Campbell, PhD, co-author of the NYTimes bestselling book The China Study, who serves on PPC’s Advisory Board. Dr. Campbell is the Jacob Gould Schurman Professor Emeritus of Nutritional Biochemistry at Cornell University, and a bio/nutritional researcher with over 60 years of experience in the field of nutritional science.
References
- U.S. Department of Health and Human Services. Bone Health and Osteoporosis: A Report of the Surgeon General. Rockville, MD: U.S. Department of Health and Human Services, Office of the Surgeon General; 2004.
- To meet the current Recommended Daily Allowance (RDA) of calcium, women ages 18 to 50, and men ages 18 to 70 need 1,000 milligrams (mg) of calcium. (https://americanbonehealth.org/nutrition/guidelines-calcium-vitamin-d-supplementation/)
- During exposure to sunlight 7-dehydrocholesterol in the skin absorbs UV B radiation and is converted to previtamin D3 which in turn isomerizes into vitamin D3. (https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3897598/)
- A recently published government bulletin from the USPSTF (U.S. Preventive Services Task Force), April 2018, concluded “that the current evidence is insufficient to assess the balance of the benefits and harms of vitamin D and calcium supplementation, alone or combined, for the primary prevention of fractures in men and premenopausal women”…or in “community dwelling, postmenopausal women.” (https://jamanetwork.com/journals/jama/fullarticle/2685995)
- Dr. Tomas Campbell, MD, recommends a vitamin D supplement of 600IU a day for adolescents and adults during the winter months. https://nutritionstudies.org/shining-light-vitamin-d/
- In this study of more than 61,000 women and 45,000 men who were followed for more than 20 years, there was a cow’s milk dose-dependent relationship: In the women studied, the greater reported milk consumption correlated with a higher mortality and fracture rate. In the men studied, the greater reported milk consumption correlated with a higher mortality rate. The study made two important conclusions related to fracture rate and mortality: 1) higher milk consumption had an association with biomarkers for oxidative stress and inflammation; and 2) milk is the main dietary source of d-galactose. In animal studies, even small doses of d-galactose were shown to cause oxidative stress, leading to chronic inflammation, decreased immune response, and reduced life span. (K. Michaelson, A. Wolk et al. BMJ 2014:349)
- Feskanich D, Willett WC, Stampfer MJ, Colditz GA. Milk, dietary calcium, and bone fractures in women: a 12-year prospective study. Am J Public Health 1997;87:992–7.
- Owusu W, Willett WC, Feskanich D, Ascherio A, Spiegelman D, Colditz GA. Calcium intake and the incidence of forearm and hip fractures among men. J Nutr 1997;127:1782–7.
- Hannan MT, Felson DT, Dawson-Hughes B, et al. Risk factors for longitudinal bone loss in elderly men and women: the Framingham Osteoporosis Study. J Bone Miner Res 2000;15:710–20.
- Cummings RG, Cummings SR, Nevitt MC, et al. Calcium intake and fracture risk: results from the study of osteoporotic fractures. Am J Epidemiol 1997;145:926–34.
- Michaelsson K, Holmberg I, Mallmin H, et al. Diet and hip fracture risk: a case-control study. Study Group of the Multiple Risk Survey on Swedish Women for Eating Assessment. Int J Epidemiol 1995; 24:771–82.
- Turner LW, Hunt S, Kendrick O, Eddy J. Dairy-product intake and hip fracture among older women: issues of health behavior. Psychol Rep 1999;85:423–30.
- Burger HG, de Laet Dacle PI, Weel AE, Witteman JC, Hofman A, Pols HA. Risk factors for increased bone loss in an elderly population: the Rotterdam Study. Am J Epidemiol 1998;147:872–9.
- https://academic.oup.com/ajcn/article/74/5/571/4737376
- https://www.hindawi.com/journals/bmri/2018/4840531/ https://orthoinfo.aaos.org/en/staying-healthy/exercise-and-bone-health/
https://www.health.harvard.edu/staying-healthy/slowing-bone-loss-with-weight-bearing-exercise